An anastomotic aneurysm after an open repair of an aortic aneurysm is always a surgical challenge. We dealt with a 65-year-old male who had a large anastomotic aneurysm on a previous AAA open repair graft, on its distal anastomosis. The size of the aneurysm was 12 cm. The patient had a right limb thigh amputation some years ago, and he was obese. He also had a history of COPD.
On the preop CT scan the size of the aorta at the level of the renal arteries was 5.5 cm and the right common iliac artery was chronically occluded (thus, probably, the right limb amputation). The left common iliac artery was diffusely stenotic by calcified plaques and the right renal artery was occluded. His preop creatinine was 1.5 mg/dl. On top of those, the patient had a retro-aortic left renal vein.
On the preoperative MDT meeting the possible solutions were two:
- Aorto-uni-iliac endograft from the aortic graft to the left common iliac artery. This solution was excluded due to two reasons. First, the size of the existing aortic graft was around 36 mm in diameter and no such endograft was available on an urgent solution (the patient had been considered as an urgent case). Possibly a custom-made endograft might had been a solution but it would need quite a long-time to be prepared. The second reason that precluded the endovascular solution was the poor iliac axis due to severe atheromatosis. The iliac axis was considered unfriendly to accommodate any endograft delivery system
- Open repair with a graft from either the previous aortic graft or the aorta above it to the left common iliac artery.
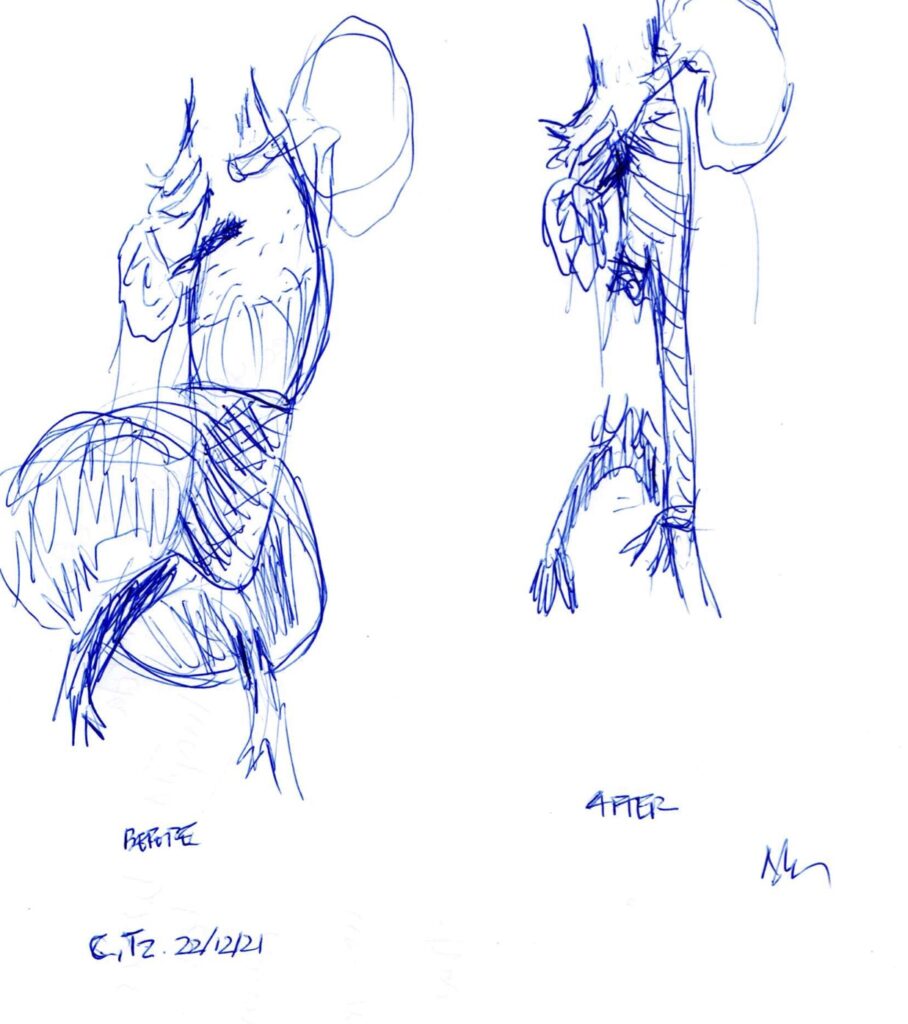
We chose the second solution. Through a left retroperitoneal incision, the aorta up to the diaphragm was exposed as well as the left common iliac artery. The left retroaortic renal vein was carefully preserved and dissected free from the underlying aneurysm sac. The aorta was cross-clamped above the celiac artery, the aneurysm sac was opened underneath the left renal vein. The previous graft was explanted. A 20/10 bifurcated graft was anastomosed proximally on a beveled fashion (like a Type IV TAAA repair) including the orifices of all three splanchnic vessels (excluding the right renal artery which was chronically occluded). The graft was passed under the left renal vein. The left limb of the bifurcated graft was anastomosed end-to-end to the left common iliac artery. The right limb was divided and double-sutured close to its orifice. This way, a customized conical graft (20 mm proximally, 10 mm distally) was created. The time of splanchnic ischemia was 58 min. The procedure is depicted in the following image.
After the procedure, the patient went to the ITU where he stayed intubated until the next morning (about 18 hours), when he was extubated. Overall, he remained in hospital for 5 days, thereafter he was discharged. His postop creatinine level climbed up to 3 mg/dl, following a gradual fall onto his preop levels.
